
When it comes to scoliosis, there are three main classifications: neuromuscular, congenital, and idiopathic. Neuromuscular scoliosis (NMS) is a type of scoliosis that occurs in individuals with conditions that affect the muscles and / or connective tissues that support the spine. It is the second most common spinal deformity, with idiopathic scoliosis being the most common.
A diagnosis of neuromuscular scoliosis can be scary, and it’s important to work with medical professionals to help you navigate your diagnosis. Throughout this article we will discuss the complexities of NMS and shed some light on your alternative non-invasive treatment options.
According to the American Academy of Orthopaedic Surgeons, “NMS is caused by an underlying medical condition that affects either the body's neurological system or muscular system—or a combination of both.” [1]
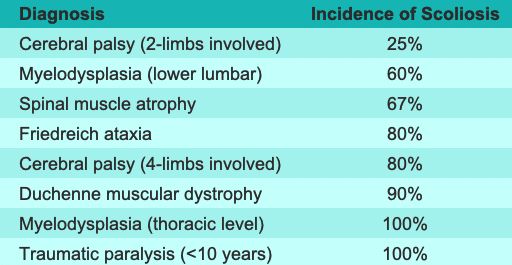
The severity and progression of NMS is related to the extent of nerve and muscle involvement associated with the individual’s neuromuscular condition. While not everyone with a neuromuscular condition develops scoliosis, it is quite common. Scoliosis Research Society created the table below to show the incidence of scoliosis based on the diagnosis.
NMS curves tend to progress rapidly and often continue to progress after skeletal maturity - well into adulthood.
Related: ICD 10 Coding for Neuromuscular Scoliosis & More
For patients with NMS who are able to walk (ambulatory), the signs and symptoms associated are similar to those associated with idiopathic scoliosis and include:
For patients in wheelchairs (non-ambulatory), NMS may cause significant changes to their appearance and interfere with daily functions. Non-ambulatory patients see:
When it comes to treating NMS, there are two approaches to treatment - surgical and nonsurgical.
Some experts say that bracing is the only non-operative treatment option available. [3] However, non-operative management of NMS often includes observation and rehabilitation in addition to bracing for the less severe cases. [4] NMS cases are typically the most difficult scoliosis cases to treat because there are significant limitations because of the underlying neuromuscular condition.
It is very important to find a highly trained doctor who has experience treating NMS. Not all CLEAR-certified doctors have experience with NMS cases. We highly recommend that patients reach out to a doctor to learn more about their experience with NMS and the different neuromuscular conditions they have worked with.
A CLEAR-certified doctor with experience treating NMS can modify some of the exercises used within the CLEAR approach to meet the needs of the NMS patient.
It is important to understand that there is no resolution to NMS. Treatment is all about properly managing the case. A doctor should set realistic expectations for the patient prior to implementing a treatment plan. If a case isn’t handled appropriately, it could lead to surgery.
Surgical treatment is often recommended for more severe cases of NMS. The American Academy of Orthopaedic Surgeons states the most common indicators for surgery with NMS patients include:
Since NMS is present due to an underlying condition, the underlying condition must be the guiding force of the treatment plan. All cases of NMS are different based on the type of neuromuscular condition the patient has.
With certain neuromuscular conditions, scoliosis may appear at a very young age. When this happens, the patient's growth must be taken into consideration when contemplating a surgical treatment approach. Many operations that stabilize the spine also stop growth in that area. When a patient is still growing, growing rods that can be lengthened with a less invasive procedure every six to nine months are typically recommended.
Scoliosis surgery is a major procedure with a high rate of complications and many side effects. One study found that, “patients diagnosed with NMS had the highest surgical-site infection rate at 13.1%.” [5] The decision to get such an invasive procedure should not be taken lightly nor made without first considering all options.
There is no resolution to NMS; treatment is all about properly managing the case. Non-surgical treatment for less severe cases of NMS includes observation and rehabilitation, in addition to bracing. A CLEAR-certified doctor with experience treating NMS can modify some of the exercises used within the CLEAR approach to meet the needs of the NMS patient.
More severe cases of NMS are often recommended for surgery; however, the decision to get such an invasive procedure should not be taken lightly without considering all options, as scoliosis surgery has a high rate of complications and many side effects.
Since NMS is present due to an underlying condition, the underlying condition must be the guiding force of the treatment plan.
[1] Diseases & Conditions Neuromuscular Scoliosis
[3] Neuromuscular Scoliosis: Current Concepts
[4] What's New in the Management of Neuromuscular Scoliosis
Disclaimer: The author’s views are his or her own and may not reflect the views of CLEAR Scoliosis Institute.

CLEAR provides a unique and innovative way of understanding scoliosis. Sign up to receive facts and information you won’t find anywhere else.
Great Newsletter on NMS!