While disc herniation and nerve compression often occur together, they can also develop independently of one another. Disc herniation can cause a pinched nerve, but a pinched nerve won't cause disc herniation, and nerve compression can also have several other causes.
A pinched nerve in the back involves excessive pressure (compression) impacting the nerve's function, and a herniated disc involves structural changes to the intervertebral disc as its inner nucleus pushes through a tear in its outer annulus.
Before comparing disc herniation and pinched nerves, let's first talk generally about the importance of healthy intervertebral discs and spinal nerves.
A healthy spine is key to quality of life; it helps us stand upright, maintain good posture, enables flexible movement, protects important organs and the spinal nerves, and facilitates brain-body communication.
The spine has many moving parts; its main structures include its vertebral bodies (bones), intervertebral discs, spinal nerves, and supportive ligaments.
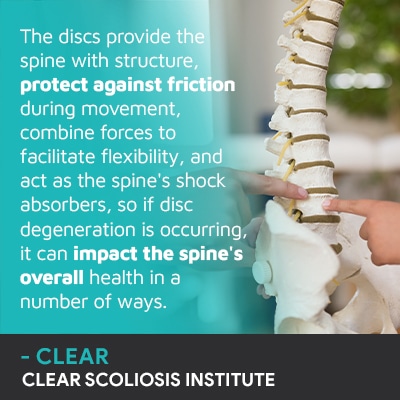
The spinal discs are key to overall spinal health because they have many functional roles.
The spinal cord consists of 31 pairs of spinal nerves, and the health of the spinal cord shapes brain-body communication as the brain and spine work together to form the central nervous system.
The central nervous system is the body's vast communication network, and the nerves are essential for healthy movement, sensation, and a number of automatic functions such as breathing and digestion.
The spine has three main sections, and disc herniation and nerve compression can happen in any section: the cervical spine (neck), thoracic spine ( middle/upper back), and the lumbar spine (lower back).
Poor disc and/or nerve health can impact overall health and quality of life.
While a pinched nerve can't cause a herniated disc, a herniated disc can cause nerve compression (pinched nerve), so let's start with how disc herniation occurs.
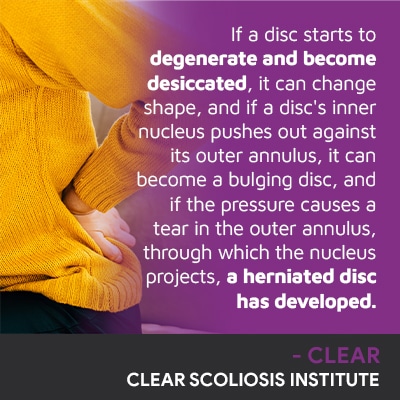
The discs have two main structures: a soft gel-like interior nucleus and a durable outer layer known as the annulus.
A healthy disc will be hydrated and its inner nucleus will maintain a central position inside the disc.
The discs are the largest structures in the body that don't have their own vascular supply, so damage can be difficult to repair and/or reverse.
When we're born, the discs are largely made up of water, but fluid levels change over time, and excessive fluid loss can disrupt a disc's health and is known as disc desiccation.
A herniated disc can cause a number of issues from mobility issues to back pain and nerve pain caused by compression.
If a disc herniates and its inner material is projecting into its surroundings, it can place excessive pressure on nearby nerves, causing a variety of symptoms.
Symptoms of disc herniation will vary based on severity, cause, and location.
Common symptoms include pain and numbness, tingling, muscle weakness, and pain that radiates into the arm or leg.
Radiating pain caused by compression can be felt far from its source, so it's important to determine the cause and location of nerve compression.
Disc location will shape a lot of its symptoms; for example, a herniated disc in the lower back can cause sciatic nerve pain because the sciatic nerve starts in the lower back.
If the lumbar spine's unnatural curve and twist is putting pressure on the sciatic nerve, it can become irritated, inflamed, and cause symptoms felt anywhere along the nerve's extensive posterior pathway.
So a herniated disc causing nerve compression in the neck is going to cause symptoms that involve the neck, shoulders, and arm, while nerve compression in the lower back is going to largely affect the lower body.
So as you can see, a pinched nerve can't cause a disc's inner nucleus to push through its outer annulus, but a herniated disc can certainly compress its surrounding tissues and nerves.
A pinched nerve isn't given the space it needs to function optimally and transmit signals, and if left untreated, nerve damage can occur, and nerve damage can be difficult to improve and/or reverse.
When it comes to treating a herniated disc, the first step is determining its underlying cause and customizing a treatment plan accordingly.
Common causes of a herniated disc include degenerative disc disease, lifestyle factors, injury, and/or the presence of an underlying spinal condition like scoliosis.
The discs are generally the first spinal structures to experience degenerative changes, and this commonly involves an excessive loss of fluid, the disc becoming dehydrated, changing shape, and adding uneven pressure that can cause a bulging and/or herniated disc.
Treatment for degenerative disc disease can include physical therapy and chiropractic care.
When lifestyle factors such as obesity and low-activity levels are contributing to poor disc health, physical therapy and lifestyle guidance can help.
If an overuse injury is the cause, the injury needs to be addressed.
Scoliosis affects close to seven million people in the United States alone, and as a progressive condition, the sooner treatment is started, the better.
Potential effects of scoliosis include postural changes such as uneven shoulders and hips, mobility and balance changes, muscular imbalance, and back, muscle, and nerve pain.
A spinal condition like scoliosis can increase the likelihood of disc herniation because the spine's unnatural bend and twist can expose the discs in the affected area to uneven pressure and wear capable of causing disc degeneration, and for older patients who are no longer growing, scoliosis is compressive.
Radiating pain is the main symptom of adult scoliosis, and as scoliosis is progressive, effects involving the discs and pinched nerves can worsen over time, and to relieve symptoms, scoliosis, as the underlying cause, has to be addressed.
Scoliosis treatment is customized and can involve a combination of scoliosis-specific chiropractic care, rehabilitative exercise, and corrective bracing.
When it comes to disc herniation and pinched nerves, there can be many causes from scoliosis to a bulging disc, spinal stenosis, and bone spurs; any type of change that means less space in the spinal canal can add pressure to nerves within and where they exit the spine.
Treatment for a pinched nerve will focus on relieving pressure, and this is commonly worked towards through condition-specific chiropractic care and physical therapy.
Overall spinal health is shaped by the health of its intervertebral discs, and nerve health is also important.
The discs give the spine structure, flexibility, prevent friction during movement, and facilitate its ability to evenly absorb/distribute mechanical stress.
If a disc starts to degenerate, it can have a number of effects, particularly in its surrounding area.
While a pinched nerve can't cause a herniated disc, a common symptom of disc herniation is nerve compression, and if a nerve is compressed inside the spinal cord, or at the nerve root where it exits the spine, symptoms can be felt in the back and/or anywhere along the affected nerve's pathway.
Pinched nerves can also develop due to bulging discs, scoliosis, bone spurs, and spinal stenosis.
Treatment options for a herniated disc can include physical therapy, chiropractic care, and lifestyle guidance, and if an underlying condition like scoliosis is causing nerve compression and/or disc degeneration, the scoliosis needs to be addressed proactively to prevent further disc and nerve damage.
A compressed nerve requires pressure-relief to reduce/alleviate its symptoms.
Here at the CLEAR Scoliosis Institute, patients experiencing nerve pain are given a comprehensive physical examination/assessment including posture, mobility, and strength, and X-ray imaging is often necessary for a complete picture of what's happening in the spine.

CLEAR provides a unique and innovative way of understanding scoliosis. Sign up to receive facts and information you won’t find anywhere else.